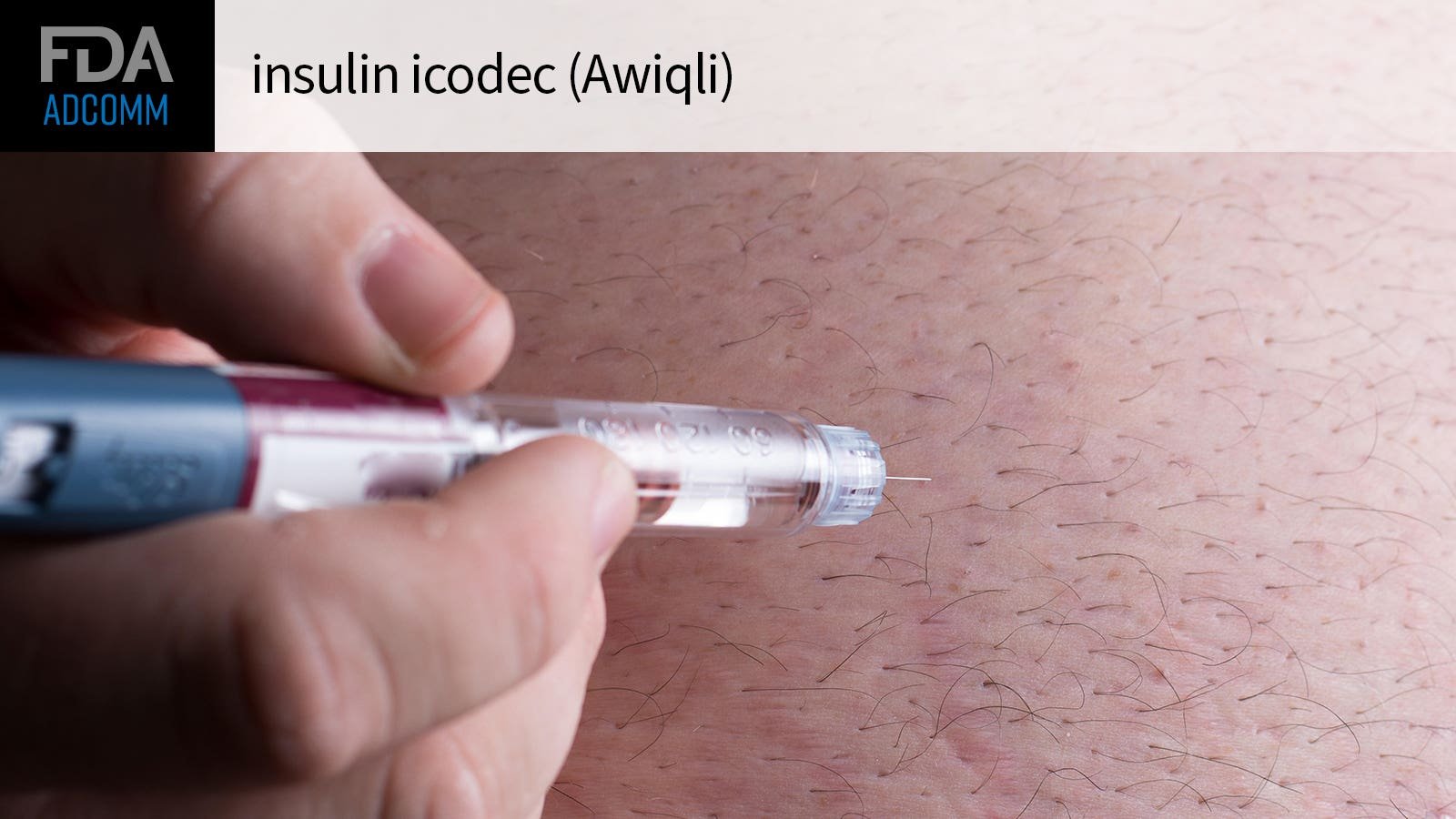
Concerns over hypoglycemia risk with an investigational once-weekly insulin product in patients with type 1 diabetes prompted the FDA to call an advisory committee together to weigh in on the matter.
On Friday, the Endocrinologic and Metabolic Drugs Advisory Committee will discuss the long-acting insulin icodec by Novo Nordisk, which is seeking an indication for improving glycemic control in adults with both type 1 or type 2 diabetes.
In the phase IIIa ONWARDS 6 trial, insulin icodec was just as efficacious — but not superior to — once-daily insulin degludec in type 1 diabetes, yielding a comparable reduction in HbA1c by week 26 (-0.47% vs -0.51%). Both insulins were used in combination with three daily mealtime insulin injections.
However, there was a significantly higher estimated rate of severe or clinically significant hypoglycemia with insulin icodec, marked by a blood glucose under 54 mg/dL (19.93 events per patient year vs 10.37 with the once-daily insulin). The highest risk period for hypoglycemia was around the time of its peak glucose-lowering effect on days 2 to 4 after injection.
This will be the main point of debate for the advisory committee, as briefing documents stated that while hypoglycemia is “an expected adverse reaction” with exogenous insulin, insulin icodec in type 1 diabetes patients in this trial showed “excess hypoglycemia … without evidence of any additional glycemic control or other benefit.”
The FDA previously told Novo Nordisk during an end-of-phase II meeting that meeting the prespecified noninferiority margin (HbA1c at 6 months) “would not be sufficient to establish a favorable benefit-risk profile” when taking into consideration the risk of hypoglycemia. At that meeting, the FDA recommended the phase III study include a third arm evaluating insulin icodec dosed twice-weekly and assess the possible need for additional bolus dose adjustments.
Novo Nordisk already proposed a few label suggestions and risk-mitigation strategies for type 1 diabetes patients that will be discussed on Friday. First, it was suggested insulin icodec be limited to type 1 diabetes patients wearing a continuous glucose monitor and those without a history of hypoglycemia unawareness or recurrence. This was the same criteria used in the trial. It also suggested that the labeling restrict use to type 1 diabetes patients whose glycemic variability is less than 36% prior to initiation.
Another proposal was an alternative dose titration strategy for this group, like cutting the bolus insulin dose by around 30% between days 2 to 4 when hypoglycemia risk is highest.
During the meeting, hypoglycemia risk will be weighed against the unmet need for a wider range of insulin options for this patient population.
Currently, all basal insulin products on the market are designed for daily dosing, so the main benefit of this product is the convenience of a once-weekly dosing option. This strategy may also help to combat nonadherence to insulin therapy — a risk factor for hyperglycemia and diabetic ketoacidosis. One recent meta-analysis found that adherence to insulin therapy in adults with type 1 diabetes was fairly low, at around 53%.
ONWARDS 6 was the only trial in the clinical program to include type 1 diabetes patients, as the other five trials only enrolled type 2 diabetes participants. In the ONWARDS 1 trial presented at last year’s American Diabetes Association meeting, there was a significantly greater average reduction in HbA1c with icodec compared with glargine U100 in insulin-naive people with type 2 diabetes. In this patient population, there was a numerically higher rate of clinically significant or severe hypoglycemia: 0.30 events per person-year of exposure with icodec and 0.16 events per person-year of exposure with glargine U100 at week 52.
“Insulin is insulin,” lead investigator Julio Rosenstock, MD, of Velocity Clinical Research at Medical City in Dallas, said at the meeting. “When we use insulin, there always will be hypoglycemia, but we only had less than one event per year.”
In March, the European Medicines Agency’s advisory committee recommended Novo Nordisk’s insulin icodec for approval in both type 2 and type 1 diabetes, though it said that the product “should only be used in patients with type 1 diabetes for which a clear benefit of a once-weekly administration is expected,” given the hypoglycemia concerns.
While the FDA isn’t required to follow its advisory committees’ recommendations, it typically does.
Kristen Monaco is a senior staff writer, focusing on endocrinology, psychiatry, and nephrology news. Based out of the New York City office, she’s worked at the company since 2015.
![Trump says he is “very positive and [open-minded] to cryptocurrency companies,” advocates for US leadership in crypto industry](https://oeisdigitalinvestigator.com/wp-content/uploads/2024/05/1146-trump-says-he-is-very-positive-and-open-minded-to-cryptocurrency-companies-advocates-for-u6653d857db444.jpg)